A 30-year-old woman in the United States was told by doctors she had parasites in her brain after presenting to the hospital with a burning sensation in her feet.
The worms seem to have been unlucky souvenirs the woman unknowingly picked up while traveling in Thailand, Japan, and Hawaii.
Embedded in her central nervous system, the quiet invaders didn’t ‘make a peep’ until 12 days after the woman had returned home. Only then did their presence cause an intense immune response that took a further week to diagnose.
Over several days, hot pain in the woman’s feet crawled up her legs, trunk, and arms, before erupting in a splitting headache that even frequent doses of pain relief medication couldn’t alleviate.
frameborder=”0″ allow=”accelerometer; autoplay; clipboard-write; encrypted-media; gyroscope; picture-in-picture; web-share” referrerpolicy=”strict-origin-when-cross-origin” allowfullscreen>
An initial visit to the emergency department turned up only a mild increase in disease-fighting white blood cells. But after days of unrelenting discomfort and a mild fever, the woman returned to a different hospital looking for answers.
Following treatment with intravenous anti-inflammatories and an anti-anxiety medication called lorazepam, her headache finally abated and she was discharged.
Once again, the symptoms persisted.
The next morning, when the woman woke, she began to pack for a vacation that she had not planned. Her roommate noticed her strange behavior and encouraged her to lie back down in bed. Hours later, when the woman was still showing signs of confusion, her partner took her to hospital.
“The development of confusion in this patient with sensory symptoms, headache, and possible intermittent fever suggests the possibility of encephalitis and further increases concern about a central nervous system infection,” explains infectious disease specialist Joseph Zunt from the University of Washington.
Testing her blood, her doctors found no sign of parasites, and a CT scan of her head showed no red flags beneath her skull. Yet when medical staff performed a lumbar puncture, they found the patient’s cerebrospinal fluid (CSF), which bathes the brain and spinal cord, contained markers of eosinophilic meningitis – a rare form of brain infection that can be caused by parasites.
Based on the patient’s recent travel and her symptoms, her doctors agreed she met the criteria for a presumptive diagnosis of angiostrongyliasis.
This insidious disease is also known as rat lungworm because it is caused by the parasite Angiostrongylus cantonensis, which starts its life cycle in the lungs of a rodent before spreading to slugs and snails.
Most people aren’t eating uncooked slugs or snails, but if we bite into a fresh, leafy vegetable that one of these creatures has slimed, the parasite’s larvae can end up in our bodies without us knowing it.
That’s one of the reasons why washing green produce is so important when staying in parts of the world where rat lungworm spreads, including Southeast Asia, the Pacific Islands, and Australia. Undercooked crab or prawns can also be a vector, as these animals eat slugs and snails, too.

When the parasites infect human bodies, they can migrate to the pulmonary arteries, swimming into the central nervous system and threatening the life of the host.
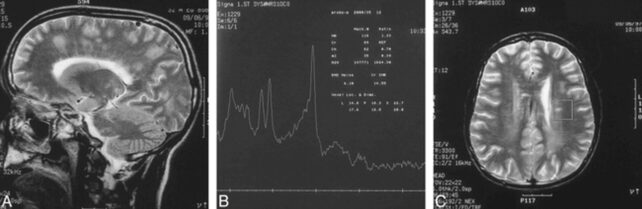
Only occasionally are the larvae able to be seen in the brain for a definitive diagnosis. Usually, brain scans only hint at damage from these parasites. The image below, for instance, shows clear signals of lesions in parts of a 32-year-old’s brain that are indicative of angiostrongyliasis.
Thankfully, the woman in the US had her brain saved from parasites by a two-week course of drugs that can cross the blood-brain barrier to treat angiostrongyliasis. The patient was also given a high dose of a steroid called prednisone to help alleviate inflammation in her brain.
Her symptoms abated with the combination treatment, and on her sixth day in hospital, she was able to go home – this time without hidden passengers in her brain.
The study was published in the New England Journal of Medicine.








Leave a Comment