A new study shows that advanced kidney disease compromises the survival of B cells and significantly reduces the immune response to the influenza virus.
B cells are a type of infection-fighting white blood cell that produces antibodies to kill microbes.
Fighting off infections when one has chronic disease is a common problem, and during the COVID-19 pandemic that scenario often turned out to be dangerous and deadly.
Comorbid health conditions are critical determinants of immune function. One comorbid condition associated with increased risk of severe infection and infection-related deaths is kidney disease. Infections are the second major cause of death in patients with kidney disease.
According to the International Society of Nephrology, an estimated 20% of patients with kidney disease die from infection. During the COVID-19 pandemic, mortality rates were as much as 10 times higher for those who had kidney disease compared to those with normal kidney function.
Lead author Partha Biswas, a professor in the microbiology and immunology department in the Renaissance School of Medicine at Stony Brook University, and colleagues, set out to better understand why those who have kidney disease are unable to mount a protective immune response. The study centered on the condition experienced during kidney disease called uremia—the accumulation of toxic metabolites in the body in the absence of kidney filtration of the blood.
To date clinical studies often show a poor B cell-mediated antibody response after an infection or vaccination in those with kidney disease. Additionally, kidney disease is a known predisposing factor for infection complications, however the reasons are not clear.
“Most studies linking kidney disease with abnormal B cell response were either performed in kidney transplant patients or are correlative in nature. Since kidney transplant patients are immune compromised, it is difficult to assess the impact of kidney disease on B cell response per se,” explains Biswas.
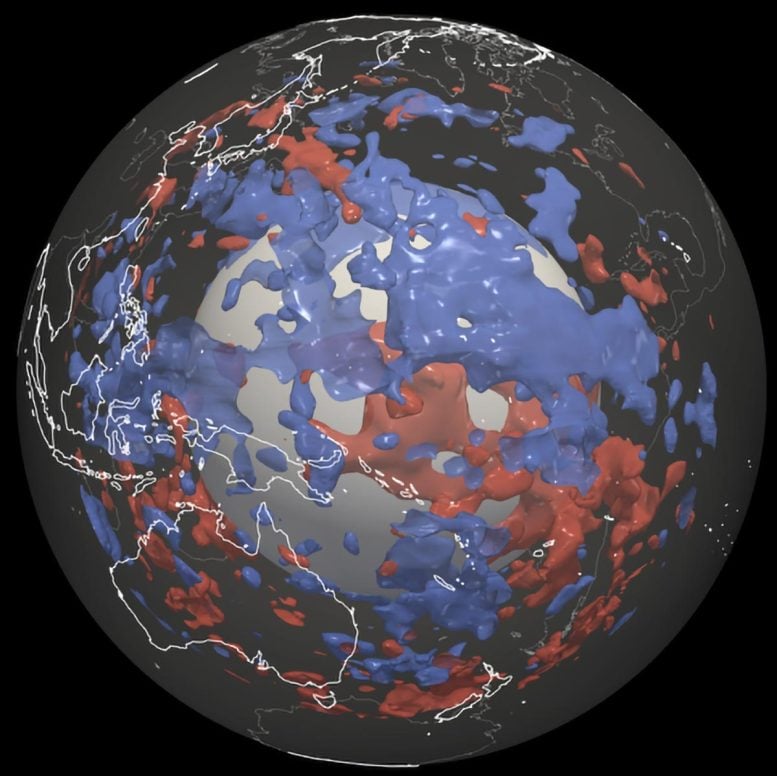
The researchers used a multiple well-characterized murine model of kidney disease that progresses to renal dysfunction in the subjects. Healthy mice and those with kidney disease were immunized with model immunogens or infected with the influenza virus to trigger a germinal center (GC) response in the spleen, which is central to the development of protective antibody level and infection-fighting response.
They discovered several cellular changes that helps to illustrate the poor immune response in the kidney disease model:
- Kidney dysfunction leading to accumulation of toxic metabolites triggered cell death in GC B cells leading to poor antibody response during immunization.
- A previously unidentified role of uremic toxic metabolites hippuric acid (HA) is responsible for increased cell death of GC B cells.
- HA drove increased death of GC B cells via activating a specific G protein coupled receptor for niacin, which appears to further affect normal B cell response.
- Kidney disease had a negative impact on and inhibits GC and antibody response following influenza virus infection.
According to Biswas, the paper provides mechanistic insights on how kidney disease negatively impacts protective B cell response infection and immunization. He and his co-investigators believe that the knowledge gained from the laboratory study may shed light on how to generate protective antibody response following vaccination in individuals with kidney disease.
Currently, Biswas and colleagues are tooling up to use this experimental system to address the apparent lack of response to SARS-CoV 2 vaccination in kidney disease individuals, which may have broader implications for other respiratory virus and bacterial infections seen in these patients.
The findings appear in Nature Communications. Collaborators included scientists from numerous departments and facilities at the University of Pittsburgh and the Medical College of Georgia.
Support for the research came in part from numerous grants from the National Institutes of Health (NIH), including several to Biswas.
Source: Stony Brook University







Leave a Comment