The first antibiotics made once-deadly infections curable, and their early developers were lauded with a Nobel. But these miracle drugs soon revealed their Achilles heel: When antibiotics are overused, they grow less effective as the bacteria they’re designed to kill evolve to have escape strategies. This flaw has prompted scientists to seek alternative solutions.
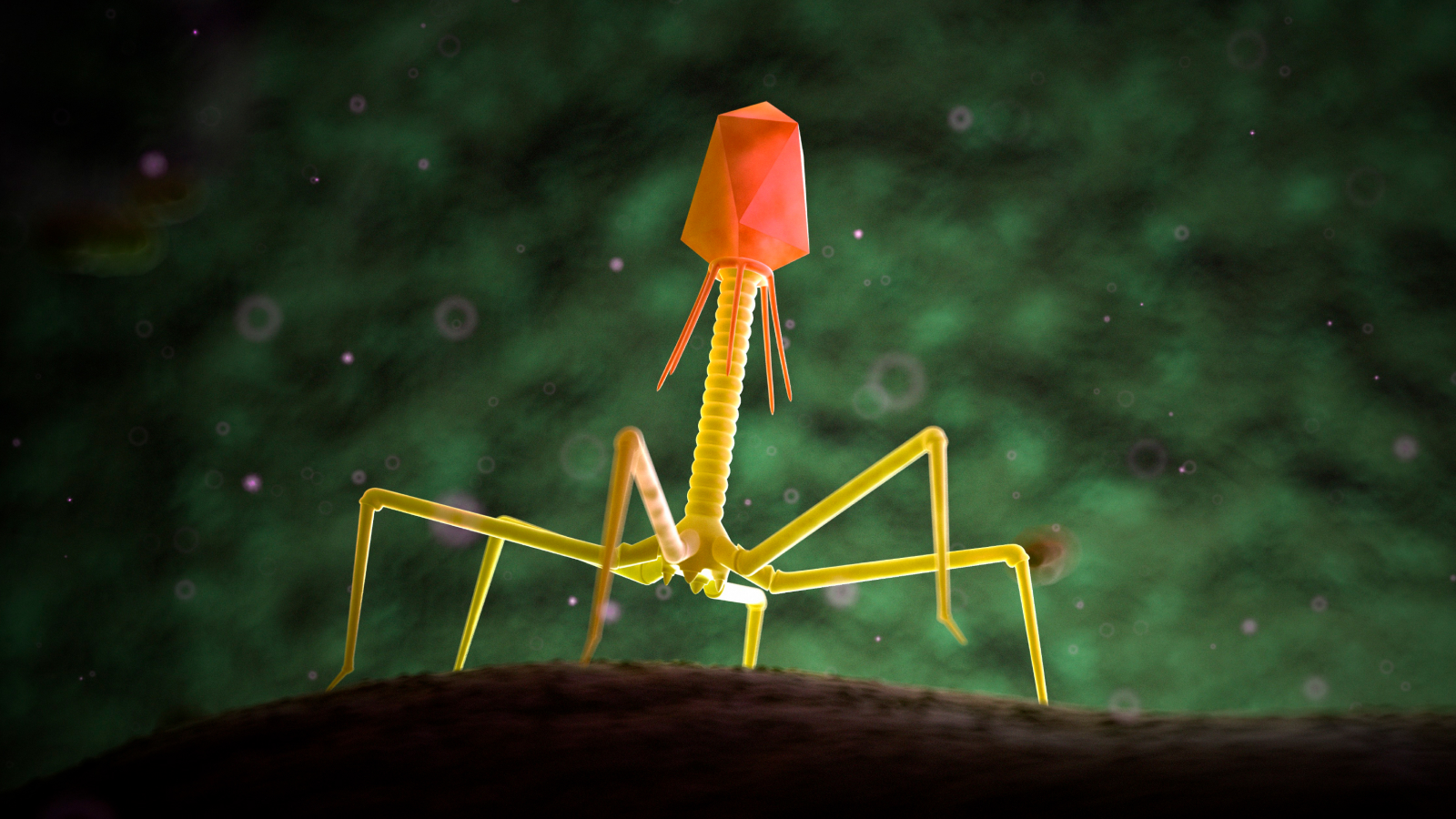
One alternative to antibiotics is phage therapy, which harnesses viruses to attack bacterial cells. Conceived over a century ago, phage therapy fell to the wayside as antibiotics rose to prominence, but recently, the field has seen a resurgence. In “The Living Medicine: How a Lifesaving Cure Was Nearly Lost — and Why It Will Rescue Us When Antibiotics Fail” (St. Martin’s Press, 2024), science journalist Lina Zeldovich recounts the complex history of phage therapy and its proponents while also highlighting how the treatment could save humanity in the future.
Related: Dangerous ‘superbugs’ are a growing threat, and antibiotics can’t stop their rise. What can?
The Phage Whisperer
Biswajit Biswas drew a syringe full of phage and injected it into his laboratory mice, one after another. The mice weren’t sick, so he wasn’t using phages as medicine. He just wanted to know how long the phages would persist inside the mice — an experiment similar to what [Giorgi] Eliava and [Félix] d’Hérelle once carried out to understand how far phages could travel in rodents’ bodies. In about a day, Biswas would test the mice’s blood to see if the phages were still floating inside them. Typically, most phages would be gone because they were quickly filtered by the liver and spleen, but sometimes a tiny fraction remained. Biswas would harvest the survivors, grow them — and inject them into the mice again.
Biswas was working on this unconventional project in the mid-1990s, in the laboratory of Carl Merril, an NIH scientist and an early phage enthusiast who was playing around with the idea of using them to treat disease. Their mice were getting blood tests right about the same time that [Alexander] Sandro [Sulakvelidze] and [Glenn] Morris were having their first phage conversations and putting together their VRE [vancomycin-resistant enterococcus] proposals. Geographically, the two teams weren’t far from each other. Both were located in Maryland. Both understood phages as medicinal agents, which the rest of the medical field viewed as nonsensical.
Merril, however, approached the problem from a different angle. Rather than treating sick mice with phages, he wanted to know how long living medicines could survive inside a creature. In humans and animals, the liver, spleen, and immune system tackle foreign invaders and filter them out quickly. Merril wanted to know how long phages could persist before they got gobbled up by the body’s natural defense mechanisms. He also wanted to know if phages could evolve to avoid being devoured. By handpicking surviving phages and reinjecting them again, Biswas and Merril hoped to find answers.
“It was a selection process,” Biswas explains. “I was growing phages and injecting them intravenously and intraperitoneally in mice, and the next day, after thirteen or eighteen hours, I would bleed the mice and take those phages and grow it again — passage after passage.” It was a method akin to what d’Hérelle outlined in his book “The Bacteriophage and the Phenomenon of Recovery,” which Eliava translated.
Originally from India, Biswas followed his family’s tradition and earned a degree in veterinary medicine. Working in animal husbandry in the mid-1980s, he watched with growing concern the increasing use of antibiotics — both to battle infections and to fatten up the animals. While looking for possible alternatives, he came across intriguing scientific literature dating back to the early 20th century, when d’Hérelle’s successful phage experiments prompted doctors to first use them to treat disease.
It’s an indictment of human beings and their greed and their misuse of things.
Carl Merril, commenting on “Arrowsmith”
Between 1930 and 1935, British medical officer Lieutenant Colonel J. Morison, who was inspired by d’Hérelle’s work, used phages during cholera epidemics in India, for treatment and prevention. In 1932, he reported few cholera deaths in the phage-treated Naogaon region, compared to 474 deaths in the Habiganj region that declined to utilize the treatment.
Related: 10 of the deadliest superbugs that scientists are worried about
“I read a paper that the British actually used bacteriophage from River Ganges to treat cholera,” says Biswas. “They inoculated a water well in a village, and that reduced the incidences of cholera.”
As a veterinarian in India, Biswas didn’t have a way to experiment with phages. But then, like Sandro, he came to the United States in the 1990s to work on his PhD. He landed in the same place as Sandro, the University of Maryland. There, he found an ally in Merril, who was equally fascinated with bacteria eaters. As an NIH scientist, Merril watched antibiotics lose their punch and knew medicine needed an alternative. “When I started my career in the 1970s, we thought antibiotics were doing fine. By the 1990s, it was clear that we were going to have a problem. I thought phages were worth trying.”
Merril had become interested in bacteriophages after taking a summer course at Cold Spring Harbor back in the 1970s. The course focused on phages’ basic biology, but for Merril, it left two big unanswered questions.
“Why don’t we use them for treating infectious diseases?” Merril asked his professor. The man told him to go read “Arrowsmith” by Sinclair Lewis — the very book that left d’Hérelle excited in the spring of 1925, shortly before he so spectacularly cured plague in Egypt. The professor’s intention was to show Merril why phages had become discredited, but that wasn’t what he found. In fact, Merril realized that his professor likely skimmed the book, if he read it at all. “He didn’t read ‘Arrowsmith,’ because if you read it really carefully, it’s not an indictment of phage,” Merril says. “It’s an indictment of human beings and their greed and their misuse of things.”
Merril’s other big question was about what happens to phages once they enter the human body — in particular, the circulatory system. Does the immune system destroy them? How quickly? Can some persist? From initial experiments with injecting phages into mice, he found that even before the immune system cells gobbled up bacteriophages as foreign organisms, the liver and spleen filtered them out. “My next question was, can we find a phage strain that wouldn’t be taken up by the liver?” he recalls. “Such a strain would be more effective.”
Merril happened to be on a committee that oversaw Biswas’s PhD research, and one day, they started talking. “I told him that I used phages before in my graduate studies to make a phage library mainly for molecular biology work,” Biswas recalls. Merril was interested. “I’d like to try to use bacteriophages to overcome antibiotic resistance problems,” he told Biswas. “Would you come work in my lab?” Biswas was intrigued. “I said, ‘It’s an interesting idea. I can work in that field.'”
For a while after he joined Merril’s lab, Biswas’s days revolved around injecting mice with phages against E. coli and Salmonella typhimurium and then taking their blood tests to see how quickly the bacteria eaters were eaten themselves, disappearing from circulation. About a day later, most phages would be gone, except for a tiny fraction. Biswas would filter them — and repeat the process again.
The first few rounds didn’t exhibit much success. But then Biswas noticed that the survivors’ numbers increased. “Surprisingly, after the eleventh round, we saw that the phage titer from the blood was getting higher,” he recalls. “So we isolated those long-circulating or long-swimming phages.” Similarly to d’Hérelle, they also turned to Greek mythology, naming their newfound potent creatures after Jason and the Argonauts, who sailed on the ship called Argo to retrieve the Golden Fleece. Although technically speaking phages can’t swim on their own, they merely float, Biswajit and Merril liked the term. “We called them Argo1 and Argo2 phages because they were good swimmers.”
The two types of Argo phages Biswas and Merril selected weren’t just good swimmers — they were exceptional. Argo1’s 18-hour survival numbers were 16,000-fold higher than the strain Biswas started with. Argo2’s was 13,000-fold higher. Notably, these Argo phages also made better medicines than their original brethren. “Mice would survive when you treat with either phage,” Biswas says. “But when we treated them with the Argo phages, they would recover much faster because the phages persisted longer in their bodies.”
From “The Living Medicine: How a Lifesaving Cure Was Nearly Lost — and Why It Will Rescue Us When Antibiotics Fail” by Lina Zeldovich. Copyright © 2024 by the author and reprinted by permission of St. Martin’s Publishing Group.






Leave a Comment