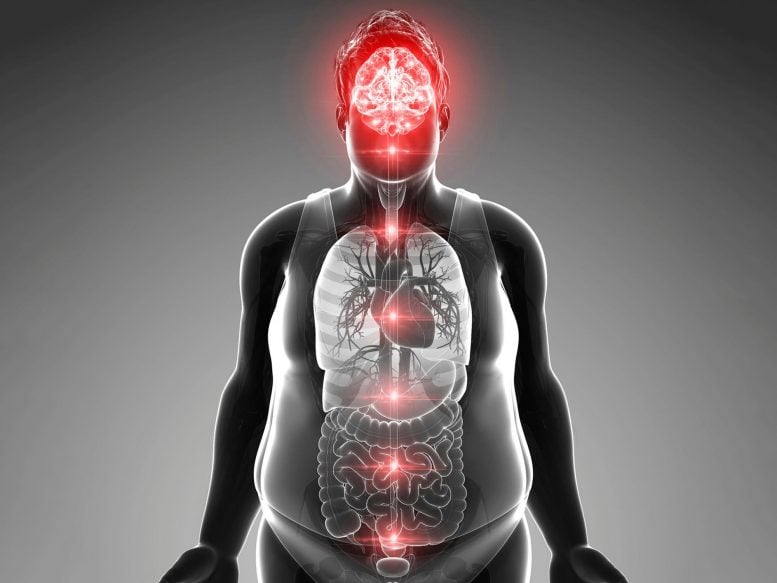
A study from Tübingen reveals that the brain plays a central role in the development of obesity.
The prevalence of obesity has increased significantly in recent decades, posing major challenges for affected individuals, healthcare systems, and medical professionals. Insulin, a key hormone, plays a crucial role in obesity’s development. Recent evidence suggests that insulin contributes to both metabolic and neurodegenerative disorders, particularly in the brain. A study conducted by the University Hospital of Tübingen, the German Center for Diabetes Research (DZD), and Helmholtz Munich provides new insights into the underlying causes of type 2 diabetes and obesity, emphasizing the brain’s role as a central regulator.
Despite its well-documented links to serious health conditions such as diabetes, heart disease, and cancer, obesity was officially recognized as a disease in Germany only in 2020. The World Health Organization has classified obesity as a global epidemic, affecting over one billion people worldwide, including nearly 16 million in Germany. Obesity is typically defined by a body mass index (BMI) of 30 or higher, with poor diet and lack of physical activity commonly cited as primary causes. However, the biological mechanisms driving obesity are far more complex than previously understood.
Obesity and the role of insulin in the brain
Unhealthy body fat distribution and chronic weight gain are linked to the brain’s sensitivity to insulin. What specific functions does insulin perform in the brain, and how does it affect individuals of normal weight? In their study, Prof. Dr. Stephanie Kullmann and her colleagues at the Tübingen University Hospital for Diabetology, Endocrinology, and Nephrology found the answer to this query.
“Our findings demonstrate for the first time that even a brief consumption of highly processed, unhealthy foods (such as chocolate bars and potato chips) causes a significant alteration in the brain of healthy individuals, which may be the initial cause of obesity and type 2 diabetes,” says Prof. Kullmann, the study’s leader.
In a healthy state, insulin has an appetite-suppressing effect in the brain. However, in people with obesity in particular, insulin no longer regulates eating behavior properly, resulting in insulin resistance.
“Interestingly, in our healthy study participants, the brain shows a similar decrease in sensitivity to insulin after a short-term high-calorie intake as in people with obesity,” says Ms. Kullmann. “This effect can even be observed one week after returning to a balanced diet,” she adds.
She is also deputy head of the Metabolic Neuroimaging department at the DZD partner Institute for Diabetes Research and Metabolic Diseases (IDM) of Helmholtz Munich at the University of Tübingen.
Focus on the brain
Prof. Dr. Andreas Birkenfeld, Medical Director of Internal Medicine IV, Director of the IDM and DZD Board Member, and the study’s final author, concludes, “We assume that the brain’s insulin response adapts to short-term changes in diet before any weight gain occurs and thus promotes the development of obesity and other secondary diseases.”
He urges more research on how the brain contributes to the development of obesity and other metabolic illnesses in light of the current findings.
Short period with far-reaching effects
29 male volunteers of average weight participated in the study and were split into two groups. For five days in a row, the first group had to supplement their regular diet with 1500 kcal from highly processed, high-calorie snacks. The extra calories were not consumed by the control group.
Both groups underwent two separate examinations following an initial evaluation. One examination was conducted immediately following the five-day period, and another was conducted seven days after the first group had resumed their regular diet. The researchers used magnetic resonance imaging (MRI) to look at the liver’s fat content and the brain’s insulin sensitivity.
Not only did the fat content of the liver of the first group increase significantly after five days of increased calorie intake. Surprisingly, the significantly lower insulin sensitivity in the brain compared to the control group also persisted one week after returning to a normal diet. This effect had previously only been observed in obese people.
Reference: “A short-term, high-caloric diet has prolonged effects on brain insulin action in men” by Stephanie Kullmann, Lore Wagner, Robert Hauffe, Anne Kühnel, Leontine Sandforth, Ralf Veit, Corinna Dannecker, Jürgen Machann, Andreas Fritsche, Nobert Stefan, Hubert Preissl, Nils B. Kroemer, Martin Heni, André Kleinridders and Andreas L. Birkenfeld, 21 February 2025, Nature Metabolism.
DOI: 10.1038/s42255-025-01226-9–





Leave a Comment